Postpartum Preeclampsia and Your Long-Term Cardiovascular Health
When Your Heart Tells a Story:
February is American Heart Month—a time when we talk about heart disease, risk factors, and prevention.
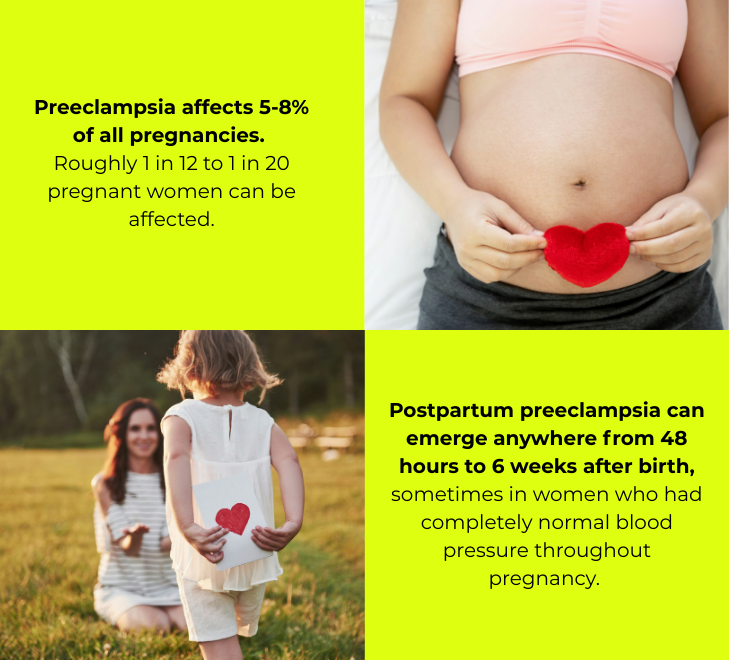
But there's one risk factor that affects millions of women and rarely makes it into the conversation: postpartum preeclampsia.
A Story We Don't Tell Enough
I experienced preeclampsia at delivery. What should have been the start of coming home with my baby turned into an extended hospital stay, a blur of magnesium drips and blood pressure cuffs, and medical teams cycling in and out of my room. The treatment itself was jarring—necessary, I understood, but disorienting during what was already a seismic event for my body. I was trying to recover from birth, trying to bond with my newborn, trying to figure out nursing—all while being monitored for a condition that felt like it came out of nowhere.
Except it didn't come out of nowhere. I knew about preeclampsia. I was educated. I had read about it, understood the risk factors, and knew it was something to watch for. And yet when it happened to me, I was shocked. There's a difference between knowing something intellectually and experiencing it in your body, in those raw and vulnerable first hours of motherhood.
Since I started speaking more openly about my experience, other women have come forward to share theirs. A friend whose sister developed it. A colleague who went through it with her second pregnancy. What strikes me in every conversation is how much the experience compounds the difficulty of an already overwhelming time. It's not just a medical complication—it's an emotional one, adding fear and uncertainty and trauma to a moment that's supposed to be about joy.
Nitasha - a friend of January Health - recently wrote and spoke about her own experience, and her words hit home. She had made it through delivery, settled in at home with her baby, and thought the hard part was behind her—only to find herself suddenly back in the hospital with a postpartum preeclampsia diagnosis. Her honesty reminded me why we need to have these conversations out loud.
And yet, when I talk to other mothers about it, so many had never heard of it until it happened to them—or didn't realize it could develop before OR after delivery. It's a diagnosis that catches many off guard, right when they're sleep-deprived, healing, and focused entirely on their newborn.
While certain factors do increase risk— i.e.: family history, or pre-existing conditions like diabetes or chronic hypertension—preeclampsia doesn't only happen to women who fit that profile. It can affect first-time mothers with no risk factors, women in their 20s and 30s who've always been healthy, women who did everything "right." That unpredictability is part of what makes it so disorienting when it happens.
But we don’t speak enough about what preeclampsia means for your health in the years and decades that follow.
What Preeclampsia Means for Your Heart—Now and Later
Preeclampsia has historically been treated as a pregnancy complication that resolves once the baby is delivered. For a long time, the medical community viewed it as something you "got through" and then moved on from. But a growing body of research tells a very different story.
The numbers are significant…
Women who have had preeclampsia face substantially elevated cardiovascular risks compared to women with uncomplicated pregnancies:
The first decade matters most
Research suggests that the window of highest relative risk is within 1-10 years after a preeclamptic pregnancy, making early intervention and monitoring particularly valuable.
These risks persist for decades.
Perhaps most striking: women over 50 with a history of preeclampsia still show doubled cardiovascular risk compared to those who never experienced the condition. This isn't a short-term elevation—it's a lifelong consideration.
Heart failure risk increases 4-fold.
A published comprehensive meta-analysis that included over 6.4 million women found that preeclampsia was independently associated with a four-times higher risk of developing heart failure later in life.
Heart attack and stroke risks are 2-3 times higher.
The same research showed a two-fold increased risk of coronary heart disease, stroke, and cardiovascular-related death. A 2023 study found that women aged 30-39 with a history of preeclampsia had five-fold higher rates of heart attack and three-fold higher rates of stroke compared to peers without that history.
Researchers are still working to fully understand the connection between preeclampsia and long-term cardiovascular disease. Two theories have emerged, and importantly, both point to the same conclusion:
Why Does This Happen?
Theory one: Preeclampsia causes lasting damage. The condition involves significant stress on your vascular system, including endothelial dysfunction (damage to the lining of blood vessels), inflammation, and changes to how your body processes lipids. Some researchers believe the body doesn't fully recover from this damage, and these changes manifest as cardiovascular disease years later.
Theory two: Preeclampsia reveals pre-existing vulnerability. Women who develop preeclampsia may already have underlying cardiovascular risk factors—subtle differences in how their bodies handle metabolic stress, inflammation, or blood pressure regulation. Pregnancy acts as a kind of "stress test," unmasking these vulnerabilities earlier than they might otherwise appear.
Here's the critical point: it doesn't matter which theory is correct. Whether preeclampsia causes cardiovascular risk or reveals it, the outcome is the same—women with a history of preeclampsia are in a higher-risk group and benefit from closer monitoring and earlier intervention.
The American Heart Association recognized this reality over a decade ago, formally including preeclampsia as a risk factor in their cardiovascular disease prevention guidelines for women. The American College of Obstetricians and Gynecologists now recommends yearly assessments of blood pressure, cholesterol, weight, and blood sugar for women with a history of early-onset or recurrent preeclampsia.
The Gap Between Guidelines and Reality
Despite these recommendations, research shows that follow-up care often falls short. One study found that while women affected by preeclampsia frequently saw their general practitioners in the years following delivery, cardiologists were consulted in only 0.3-2.4% of cases.
Part of the problem is structural: once the postpartum period ends, women often return to fragmented care—a PCP here, an annual OB visit there—with no one connecting the dots between their pregnancy history and their long-term health trajectory. The single postpartum visit at six weeks, if it happens at all, is focused on immediate recovery, not cardiovascular risk stratification for the next 30 years.
And part of the problem is awareness. Many women simply don't know that their preeclampsia diagnosis carries implications beyond pregnancy. They're not told to mention it to future healthcare providers. They're not counseled on lifestyle modifications that could reduce their risk. The conversation ends when the pregnancy ends.
What Actually Helps: Monitoring, Awareness, and Sustained Support
The good news is that cardiovascular risk isn't destiny. The same lifestyle factors that reduce heart disease risk in the general population—maintaining healthy blood pressure, regular physical activity, balanced nutrition, not smoking, managing cholesterol and blood sugar—are effective for women with a history of preeclampsia too.
But here's what makes the difference: knowing you need to pay attention in the first place.
The Monitoring Cliff After Delivery
Here's the paradox: during pregnancy, your OB monitors you closely. Blood pressure checks at every visit. Urine tests. Watchful eyes on any sign of preeclampsia developing. The medical system is built to catch it before delivery.
But the moment you leave the hospital? You're largely on your own.
Postpartum preeclampsia is at its highest risk between days 10-14 after delivery—well past the typical 48-hour hospital discharge. And it can develop anytime in the first six weeks, sometimes in women who had completely normal blood pressure throughout pregnancy and delivery. Yet most women don't have a medical appointment scheduled until that six-week postpartum visit, if they make it at all.
This means the period of greatest vulnerability is also the period of least medical oversight. Women are sent home with instructions to "call if something feels wrong," but many don't know what "wrong" looks like—especially when headaches, swelling, and fatigue all feel like normal parts of new motherhood.
And beyond those first six weeks, the monitoring gap widens further. The long-term cardiovascular implications of preeclampsia unfold over years and decades, but follow-up care rarely accounts for this. Your pregnancy history gets filed away, and the connection between that diagnosis and your heart health at 40, 50, or 60 often goes unaddressed.
Blood Pressure Monitoring Is Foundational
Blood pressure is often called a "silent" indicator because elevations frequently occur without symptoms. For women with a history of preeclampsia, regular BP monitoring isn't optional—it's essential. Research shows that women who experienced preeclampsia have significantly higher blood pressure at both 6 months and 2 years postpartum compared to women with uncomplicated pregnancies, even when readings fall within "normal" clinical thresholds.
Home blood pressure monitoring allows for more frequent tracking than periodic clinic visits and captures patterns that might otherwise go unnoticed—like elevated readings in the morning, or gradual upward trends over months.
Connection Beats Fragmentation
Bodies continue to change for months after delivery. Hormonal shifts, sleep disruption, the physical demands of caring for an infant, and the metabolic changes of breastfeeding all affect cardiovascular function. Women with a history of preeclampsia need support that extends well beyond the arbitrary six-week mark, with ongoing check-ins that track how their bodies are actually responding over time.
Perhaps most importantly, women benefit from care that connects the dots—between their pregnancy history and their current symptoms, between their blood pressure readings and their lifestyle factors, between their immediate recovery and their long-term health trajectory.
This is where fragmented care fails, and where a different model of support can make a real difference.
How January Approaches This
At January, we believe that postpartum care shouldn't end when the OB signs off. Our model is built around sustained support—not just for the first week or month, but through the full arc of recovery and beyond.
For members with a history of preeclampsia or other hypertensive disorders of pregnancy, this includes:
Blood pressure tracking as a core component of care. We provide BP cuffs to our members because we believe home monitoring shouldn't be an afterthought—it should be built into recovery from day one. Our platform helps members log readings, spot trends, and know when something needs attention.
Regular check-ins that evolve with you. Recovery isn't linear, and neither is our support. Our concierge team checks in regularly—not just to see how you're doing today, but to track how your body is changing over weeks and months, and to adjust your care plan accordingly.
Education and advocacy. We help members understand their risk factors and communicate effectively with their broader care team—including making sure future providers know about their pregnancy history.
Coordination across the full picture. Cardiovascular health doesn't exist in isolation. It connects to nutrition, sleep, physical activity, stress, and mental health. Our approach brings these threads together, so you're not managing your recovery in silos.
Preeclampsia may be a chapter in your story, but it doesn't have to define your health trajectory. With awareness, monitoring, and the right support, women can take meaningful steps to protect their cardiovascular health for decades to come.
This Heart Month, we're thinking about all the ways women's heart health gets overlooked—and all the ways we can do better. If you experienced preeclampsia or other hypertensive disorders during or after pregnancy, know that you're not alone, and your long-term health matters. If you have concerns, be sure to consult with your provider.
Learn more about how January supports postpartum recovery at january.care.
Modern motherhood deserves modern solutions.
The village isn’t gone, it’s just been reimagined.
References:
Wu P, et al. "Preeclampsia and Future Cardiovascular Health: A Systematic Review and Meta-Analysis." Circulation: Cardiovascular Quality and Outcomes, 2017. Link
Hallum S, et al. "Risk and trajectory of premature ischaemic cardiovascular disease in women with a history of pre-eclampsia." European Journal of Preventive Cardiology, 2023.
Stuart JJ, et al. "Cardiovascular Risk Factors Mediate the Long-Term Maternal Risk Associated With Hypertensive Disorders of Pregnancy." Journal of the American College of Cardiology, 2022. Link
Henry A, et al. "Preeclampsia-Associated Cardiovascular Risk Factors 6 Months and 2 Years After Pregnancy: The P4 Study." Hypertension, 2024. Link
American Heart Association. "Preeclampsia doubles women's stroke risk, quadruples later high blood pressure risk." 2014. Link
Preeclampsia Foundation. "Heart Disease & Stroke." Link
Palmiero P, et al. "Long-Term Cardiovascular Risk and Maternal History of Pre-Eclampsia." Journal of Clinical Medicine, 2025.